
Vitamin B12 Deficiency and Long COVID
Long COVID is an
emerging problem following prolonged COVID infections
Long COVID is very
similar to Post Viral Fatigue
Long COVID and Post
Viral Fatigue can be causative for Chronic Fatigue-like symptoms
Factors predisposing for Long COVID are similar to those predisposing for COVID
Critical in
recovery from Long COVID, is restoration of functional vitamin B2 sufficiency
Data suggests that
one of the predisposing factors for Long COVID is lack of Selenium
Functional B2
sufficiency is essential to restore functional vitamin B12 sufficiency The majority of the
symptoms from Long COVID come from functional insufficiency of vitamin B12. Studies are
emerging that similar, but worse symptoms can occur post mRNA vaccination
against COVID - Long Vax. The symptoms were
fatigue, brain fog, dizziness, stomach upset, heart palpitations, issues with
sexual desire or capacity, loss of smell or taste, thirst, chronic coughing,
chest pain, and abnormal movements. Another symptom was post-exertional malaise,
or worse symptoms after mental or physical exertion. Studies suggest
that there is almost a fatal attraction between COVID and the macrophage, or
more specifically an interaction between the S protein of SARS-CoV-2 with the
ACE-2 receptor on the alveolar macrophage (Wang et al, 2020),
with subsequent activation of the macrophage, which if left uncontrolled
leads to the cytokine storm, typical of the advanced disease.
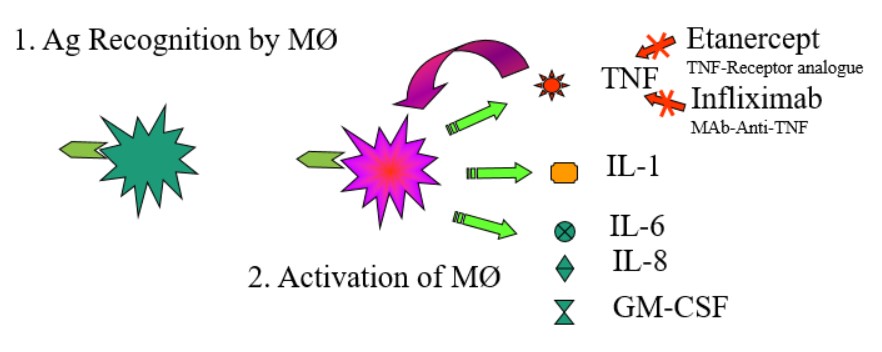
Simple model of
activation of macrophages by antigen In the simple model
of antigen activation, binding of antigen to macrophages leads to the activation
of the macrophages, and the release of inflammatory and chemotactic factors such
as TNF, IL-2, IL-6, IL-8 and GM-CSF. More recently
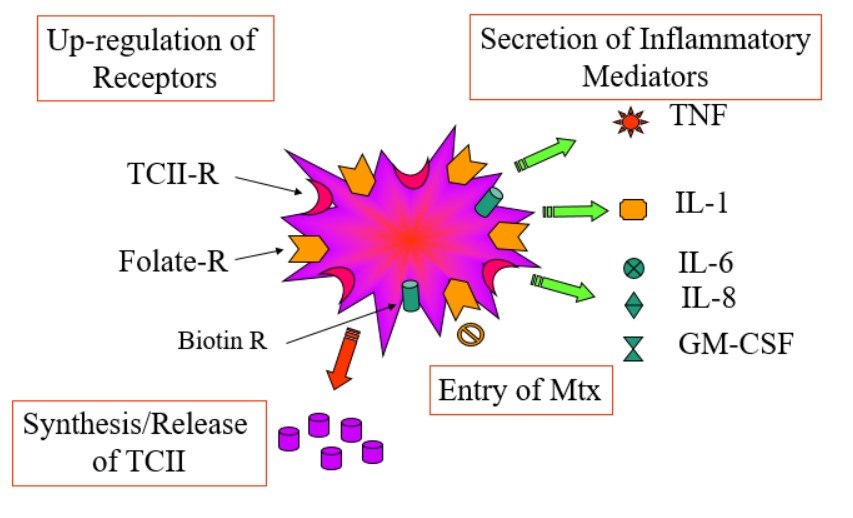
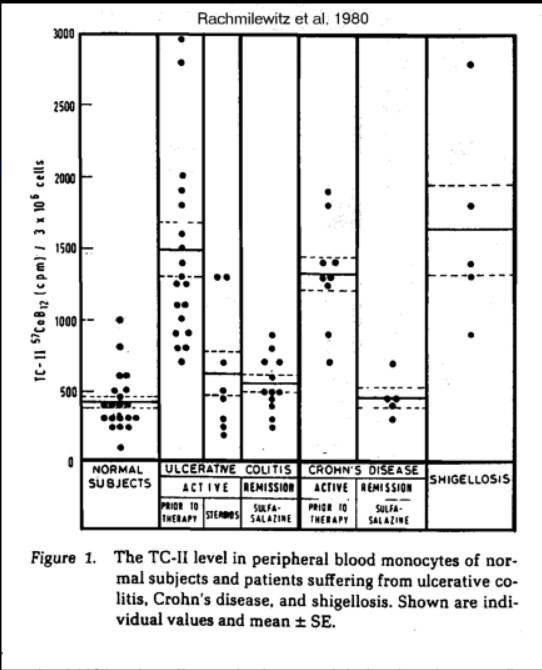
Russell-Jones, and others (personal observations 2015), it has been shown that activated
macrophages up-regulate receptors involved in the uptake of vitamin B12 (TCII-R),
the folate, and biotin (Chandrupatla .et al, 2018; Figerio et al, 2019; Moisio
et al, 2019; Jahandideh et al, 2020; Yi 2016; Muller 2007). At the time of
activation, there is massive production of transcobalamin (B12 binding protein)
by the macrophages, with up-regulation of the TCII-Receptor (Rachmilewitz et al,
1980; Seetharam 2007; Rabinowitz et al, 1982; Melmed et al, 1986).
Receptor
up-regulation in activated macrophages More
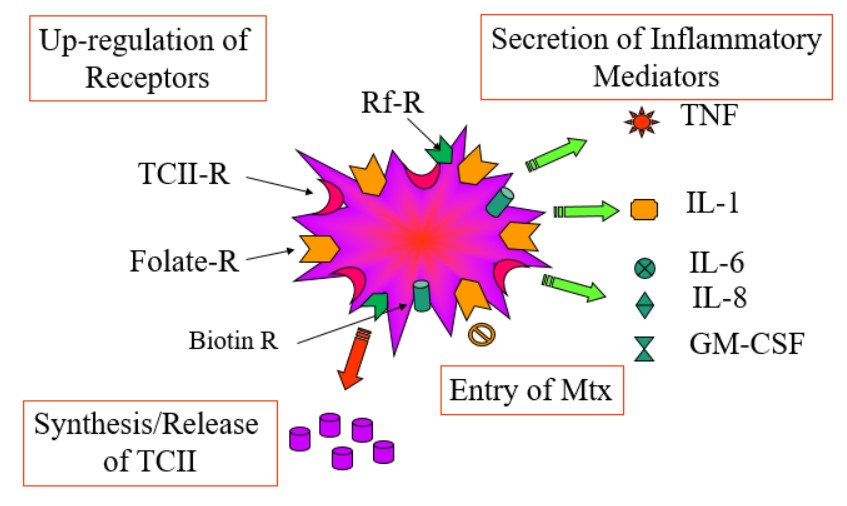
recently it has been found that there is considerable targeting of riboflavin to
activated macrophages
Riboflavin
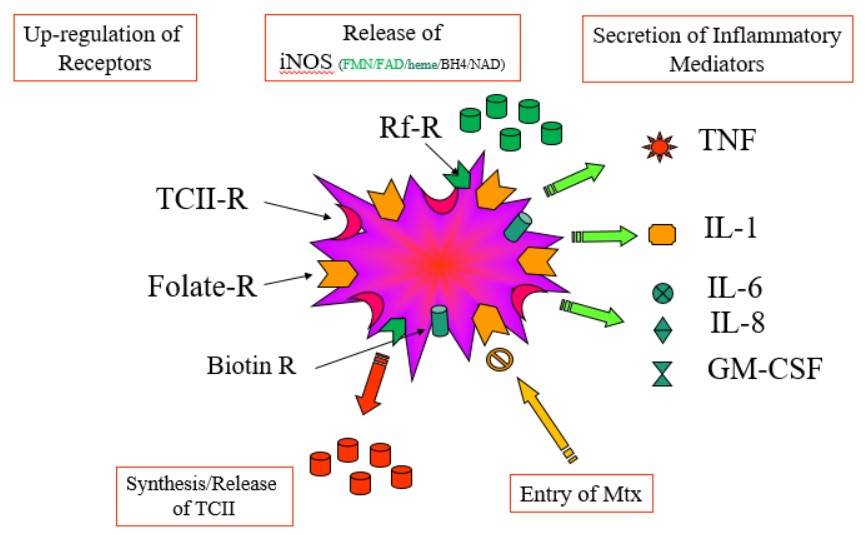
receptor up-regulation in activated macrophages Apart from
its role in the methylation cycle, riboflavin as FMN and FAD, along with vitamin
B2, BH4 and heme iron is critical for the function of Inducible NOS - iNOS,
which has a critical role in the production of the highly active reagent,
Nitrous oxide. This then is part of the inflammatory cascade in the macrophages
- the production of NO by iNOS.
Riboflavin
receptor up-regulation in activated macrophages Role of Selenium
in the Macrophage. Activation of
macrophages involves binding of Thyroid Hormone to the Macrophage, with
subsequent conversion of T4 to T3 by the
Selenium dependent enzyme iodothyronine deiodinase. In turn, activation of
riboflavin to FMN involves the action of T3 in turning on synthesis of
Riboflavin Kinase. In Selenium deficiency activation
of vitamin B2 is incomplete and hence levels of FMN and FAD would be lower
inside the cell. This would be exacerbated by the use of Selenium by the Selenoprotein, Glutathioine-Peroxidase, potentially leading to a deficiency in
the production of FMN and then FAD as part of the inflammatory cascade in COVID
infections. The high demand for
Selenium in the activation of riboflavin, in the Selenoprotein Glutathione-Peroxidase,
and in supplying active B2 for iNOS and glutathione reductase may go some way to
explaining the observation that morbidity to COVID is higher as Selenium levels
decrease. It also potentially means that there is an elevated consumption of
Selenium during the inflammatory process. Part of the
inflammatory cascade involves the activation of oxygen by NADPH Oxidase to
generate the reactive oxygen species O2**, This in turn is further activated to
generate hydrogen peroxide (H2O2). Under normal
circumstances the H2O2 is then converted to hydroxide and
then water by the Selenoprotein Glutathione-Peroxidase (GSHPx(Se). Maintenance
of REDOX potentials within the macrophage occurs by thioredoxin and the
Selenoprotein Thioredoxin Reductase. Los of activity of thioredoxin is
conditionally lethal in the embryo.
In Selenium
deficiency this reaction is reduced and so dangerous H2O2
would accumulate inside the cell and cause massive intracellular damage.
Further, the reduction of oxidized glutathione (GSSG) requires the FAD-dependent
enzyme glutathione reductase (GSH reductase). This would also be reduced in
Selenium deficiency. Control of the inflammatory process, particularly in the
lungs, involves the interaction between thioredoxin and the Selenoprotein
thioredoxin reductase. Invasion of macrophages by agents such as COVID, would be
expected to dramatically lower levels of available Selenium, and thereby
compromise the generation of FMN, but also potentially upset the formation of
Seleno-cysteine-tRNA. There are additional
problems that present in low Selenium Low Selenium, due to
it's effect on reducing activation of vitamin B2 to FAD, has the dual effect of reducing the activity of GSH-reductase,
and so the reaction GSSG => GSH will be reduced, increasing inflammation,
but also, because of the requirement for FMN and FAD in the cycling of methyl
B12, lack of FMN and FAD would lead to lower methylation and reduced production
of GSH, per se. The lower activity of the sulphation cycle in Methyl B12 deficiency
reduces the amount of GSH produced and so the greatly increased reaction of H2O2 potentially causing
death due to an over-active inflammatory response - Inflammatory storm. In functional B2
deficiency, methyl Co(II)B12 accumulates inside the cell. Nitrous oxide
reacts with the Co(II)B12 forming toxic NO-Co(III)B12, which is inactive as a
B12 analogue in the methylation cycle. The NO-Co(III)B12 can be reduced by
Cytochrome P450 (which requires heme iron and FAD), but in low FAD, this
reaction doesn't work effectively. Even if it does the product is Co(II)B12,
which will accumulate inside the FMN/FAD deficient cell due to reduced ability
of the enzyme methionine synthase reductase (MTRR), an enzyme dependent upon FMN
and FAD. The result would be the gradual build up of inactive B12 in the body,
plus the reduced production of the prime methylation product, S-Adenosylmethionine
(SAM). Lack of SAM then leads to lower production of the methylation products
CoQ10 and creatine. Continual reduction in CoQ10 and creatine then cause the
chronic fatigue associated with Long COVID. Apart from
B2/selenium/B12 and folate, the activated macrophage appears to have a huge
demand for iron, and there is a dramatic increase in serum ferritin levels post
COVID, which can be prolonged for weeks and even months post COVID, leading to
hyperferritinemia, typical of Macrophage Activation Syndrome (MAS) (Rosario et
al, 2013; Kernan and Carcillo, 2017), and eventually contribute to post viral
fatigue and a drop in the activity of the iron-sulphur protein, aconitase,
thereby adding to the fatigue.
This elevated ferritin level is typical of inflammatory diseases, serum ferritin
levels are a rather non-specific marker of the acute phase response, which is
often ignored or not measured when the patient presents acutely. In COVID
ferritin levels may be extremely high and, while not specific, these very high
levels may be helpful diagnostically (Mahroum et al, 2022; Zhou et al, 2020:
Ruscitti and Giacomelli),
2020. Despite the elevated ferritin levels, serum Haemoglobin levels were lower
in COVID patients (Raman et al, 2022;
Mohiuddin et al, 2021;
Iftikhar et al, 2021).
In many respects this is very similar to MAS (Guo et al, 2017).
Studies in COVID affected individuals, looking at
homocysteine levels, a standard marker of functional vitamin B12 deficiency,
have shown elevated homocysteine, in COVID patients, which was predictive of the
severity of the infection. This would correlate with lack of functional B2
(possibly due to Selenium usage), which would result in inactivation of vitamin
B12 in these individuals (Keskin et al, 2022; Ponti et al, 2020; Homocysteine
levels correlated with the severity of infection (Carpenè
et al, 2022; Ponti et al, 2021).
Further imaging experiments have shown considerable targeting of vitamin B12 to
macrophages, which also have been shown to release large quantities of
transcobalamin into the circulation. Data from inflammatory conditions such as
rheumatoid arthritis, ulcerative colitis, Crohn disease, and Gaucher's
disease have shown highly elevated vitamin B12 binding proteins in serum. Within
the macrophage, vitamin B12, through its role in the methylation cycle is
involved in the production of melatonin, which appears to have a role in
limiting the inflammatory response. Individuals with over deficiency in vitamin
B12, or functional deficiency in vitamin B2, would be more likely to have a
higher inflammatory response and potentially this deficiency leads to the
classical inflammatory storm seen in serious COVID infections.
Evidence suggests that in prolonged inflammation, there is sufficient reduction
in levels of Selenium to reduce the levels of FAD sufficiently that formation of
GSH is reduced such that Selenite cannot be converted to Se-CystRNA. Levels of
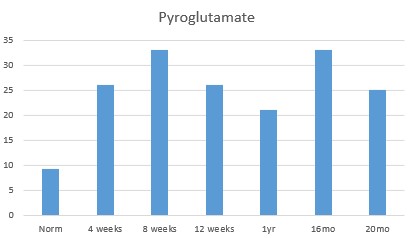
pyroglutamate rise significantly and this in turn affects the activation of
vitamin D (See Russell-Jones, 2024)
The "fight"
against COVID involves sequestration and utilization of vitamins such as vitamin
D, vitamin B2, vitamin B12 as well as iron. Levels of serum Ferritin are greatly
increased during, and following, COVID infection. Energetically huge amounts of
vitamin B2 and B12 are utilized in the "fight" against COVID, and after the infection people who recover can
have greatly depleted levels of these vitamins, and those with higher
susceptibility to the virus are likely more to suffer long term effects,
including prolonged Chronic Fatigue like symptoms - also known as Long COVID. In
addition, many have signs of prolonged reduced respiratory function, Evidence
suggests that in such cases there is a prolonged inflammatory response, which
must be resolved. Prolonged
Macrophage Activation is a consistent feature of even minor COVID infections
and seems to contribute to the development of Long COVID (Fakhri
etal, 2020; Booz etal, 2020;
Sefik etal, 2022,
Park, 2020; .Percivalle
etal, 2021) Symptoms of
Long COVID are very similar to ME/CFS, and include fatigue, brain fog,
myalgia, headache, dizziness, breathlessness, palpitations, poor sleep, anosmia and
gastrointestinal problems (McCaddon and Regland, 2021). Recovery from long
COVID therefore involves similar treatment to that for CFS. Functional B2 must
be restored, which may involve supplementation with Iodine, Selenium and/or
Molybdenum, as well as administration of high levels of vitamin B12, and vitamin
D. Long COVID is very common even in young children with up to 12% of 16-18 year
old children (Guido etal, 2022). The rate of Long COVID appears to be reduced by
50% in double vaccinated individuals (Stein etal, 2022) Fatigue is
the result of reduced production of CoQ10 and creatine, due to lower methylation
that occurs in functional vitamin B12 deficiency.. Assessment of deficiency can be achieved by Organic Acids Test (Great Plains
Laboratories), HMTA (DData), and normal blood tests, particularly TSH/T4/T3, Hb/Hct
and ferritin.
Selenium deficiency
may occur due to the need for conversion of T4 to T3 as part of the activation
of the macrophages. This then if further exacerbated by the production of high
levels of glutathione peroxidase, and the production of thioredoxin reductase. Molybdenum
deficiency may occur due to the normal innate immune mechanisms, one of which is the production
of Xanthine Oxidase, which could drain levels of Molybdenum and so exacerbate Long
COVID. Thus, Molybdenum deficiency, either due to "consumption" by xanthine
oxidase or dietary insufficiency, results in a reduced production of FAD Synthase
(Skulachev, 1998). Elevated
homocysteine correlates with the severity of COVID infections, would in turn
correlate with the potential for the development and sustenance of Long COVID. Functional
vitamin B12 deficiency, results in decreased production of CoQ10, an
essential molecule in the electron transport chain, and also a reduced
production of creatine, both of which are associated with lower energy output.
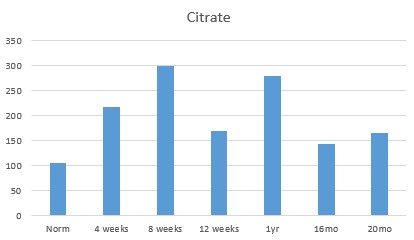
When these are combined with lower activity of the enzyme aconitase due to iron
deficiency, and lower production of FMN/FAD, then energy production from fat,
sugar and protein and reduced efficacy of the Krebs cycle and the electron
transport chain, would all result in a chronic state of fatigue Glutathione
deficiency. OAT analysis has shown extremely elevated levels of
pyroglutamate, suggesting that the extreme B12 deficiency is stopping the
synthesis of intracellular cysteine, and the subsequent production of
glutathione. This then would also reduce the ability of the macrophages to
process selenite, leading to reduced production of the protective Selenoproteins
Glutathione peroxidase, and Thioredoxin reductase. Evidence suggests
that the severity of COVID, and subsequently of LONG COVID is inversely
proportional to vitamin D levels, hence the higher the vitamin D, the less
likely that firstly there is death from COVID, but also that there will be Long
COVID (Filippo etal, 2023:
Nielsen etal, 2022;
Coronavirus: study claims vitamin D deficiency increases risk of death by
COVID-19 | news.com.au — Australia’s leading news site). One can but wonder
why the governments then proceeded to lock people inside, and not recommend that
people take vitamin D.
There is and accumulating amount of evidence that COVID infections cause
functional deficiency in vitamin B12, which can be measured by the increase in
homocysteine levels in patients (
Initial resistance to COVID-19
depends upon functional vitamin B2, iron, Selenium, vitamin D and functional
vitamin B12
Those who have
lower levels of Iodine, Selenium and Molybdenum, are at risk of developing
functional vitamin B2 deficiency, and that in turn increases the chances of
functional vitamin B12 deficiency Functional vitamin B12 deficiency
then can result in prolonged fatigue due to the reduced production of CoQ10
and creatine, with reduced energy output Long Covid or Post viral fatigue
often ensues
There is developing evidence that many people develop longer symptoms after
COVID, with up to 50% developing Post-COVID anxiety with overlapping symptoms
such as
Generalized Anxiety
Disorder
Obsessive-Compulsive
Disorder
Post Traumatic Stress
Disorder
Major Depressive
Disorder
Illness anxiety
Panic Disorder
Long COVID Symptoms
COVID and the Macrophage
Long COVID
Vitamin D and Long Covid
Functional B12 Deficiency following COVID
Long COVID and Post Viral Fatigue
Long COVID and Anxiety
Given that The "fight" against COVID involves sequestration and utilization of vitamins such as vitamin D, vitamin B2, vitamin B12 as well as iron", it would be expected that these symptoms originate from lower vitamin D and lower functional vitamin B12 levels. (https://psychcentral.com/anxiety/anxiety-after-covid#other-conditions Klaser etal, 2021; Piazza etal, 2022)
Recovery from Long COVID
Recovery from Long COVID requires restoration of functional B2, first and then restoration of functional vitamin B12 using the RnB Protocol. It is essential that functional vitamin B2 activity be totally restored or attempts to restore functional B12 deficiency will either fail or be less than optimal.(Lirysl, 3005; Liu etal, 2020; Santos etal, 2012; Chen etal, 2021; Mamun-Or-Rashid etal, 2021; Kang etal, 2020; Zhu etal, 2022; Cai etal, 2019). Of interest is the finding that vaccination offers less than 15% protection against the development of Long COVID (Reardon 2022). Further (See below) vaccination can actually induce Long Vax.
Inhibition/reduction of MAC in those with Long COVID
The current hypothesis is that if macrophages are still activated due to the uncontrolled inflammatory response it may be very hard to treat the condition, unless you can inhibit/reduce the inflammatory response. One product that has shown promise against inflammation due to influenza virus is curcumin. Another potential treatment is the use of Krill oil, which has Astraxanthin it, which has an anti-inflammatory activity on macrophages (Fakhri etal, 2022; Farruggia etal, 2018);
See https://pubmed.ncbi.nlm.nih.gov/21663638/ and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5596526/. Other approaches are using Reseratrol https://www.mdpi.com/2076-3921/11/9/1690 and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8884665/ and Pterostilbene https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7401285/ . Potentially treatment with the natural anti-inflammatory, melatonin would have benefit in reducing the inflammatory response (Bahrampour etal, 2020; Brown etal, 2021: Cross etal, 2021; Loh etal, 2022, 2023).
Altered Metabolism post COVID Vaccination - Relevance to Long Vax
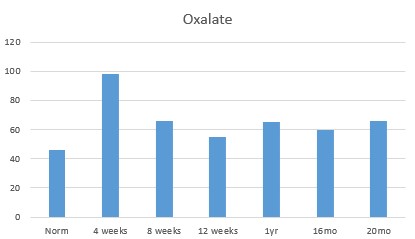
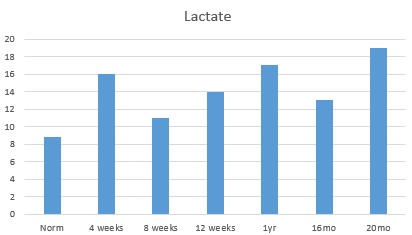
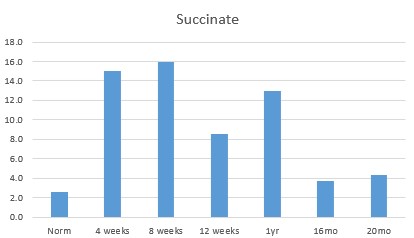
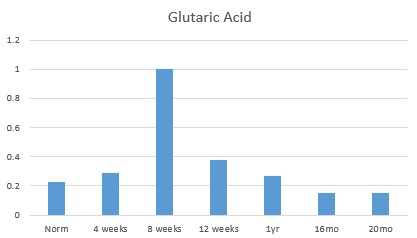
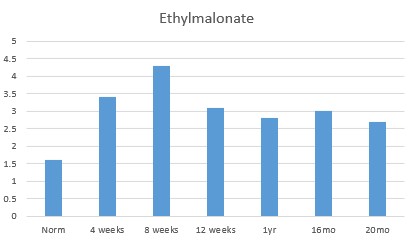
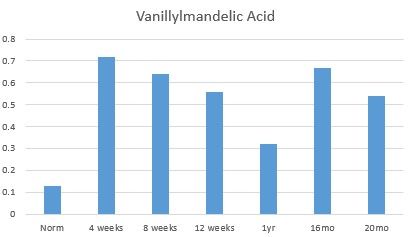
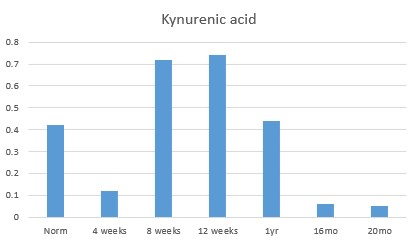
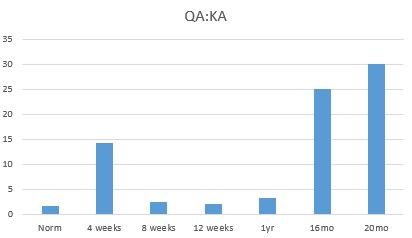
Preliminary studies using OAT data recovered before and ruing recovery from COVID-19 vaccination reveals the following deficiencies, which potentially represent that seen in Long Vax.
-
Evidence of decreased functional activity of vitamin B2 - including elevated oxalate, succinate, lactate, sebacic acid, and suberic acid.
-
Evidence of decreased functional activity of vitamin B12 - including elevated Methylmalonic acid, Ethyl malonate, Methylsuccinate (Adenosyl B12 deficiency), and elevated HVA, VMA, QA, KA and Pyroglutamate. Functional FMN deficiency, due to insufficient Iodine and of Selenium could be seen early on with the elevated QA:KA ratio.
-
Evidence of decreased functional iron deficiency could be see in the reduced activity of the iron-sulphur protein, aconitase resulting in elevated citrate..
Long COVID like sequelae post vaccination - Long Vax
There is accumulating evidence of potentially serious pathology following COVID vaccination, particularly with the PEGylated vaccines, such as Pfizer and Moderna. (I-RECOVER: Long COVID Treatment - FLCCC Alliance (covid19criticalcare.com)). This real condition has been called long vax (Loh etal, 2021, 2022: Finsterer 202A, Lee 2023' Kamoi etal, 2024) pathologists interpretation can be found at the following site
https://youtu.be/kEE5OfiVS7o. Long Vax and Long COVID frequency are so high that the whole vaccination strategy has been questioned Is it long COVID or long vax? Does the government want to know? | The Hill . Potentially the Long Vax effects also have shown up as excess deaths in 2022 (Excess deaths in 2022 among worst in 50 years (bbc.com), However, in typical fashion this concept has been squashed (Matt Canavan raised questions about what's causing Australia's excess deaths. So what is really happening? - ABC News), Excess Deaths in Australia: Frequently Asked Questions – Parliament of Australia (aph.gov.au), This is despite countless law suits against Astra Zeneca and the COVID-19 vaccine (AstraZeneca faces legal challenge over Covid vaccine (bbc.com); (BMJ 2023; 380 doi: https://doi.org/10.1136/bmj.p725 (Published 28 March 2023) (Re: Patients launch legal action against AstraZeneca over its covid-19 vaccine | The BMJ)(AstraZeneca faces two lawsuits in London over COVID-19 vaccine | Health News | Al Jazeera)(In rare cases, coronavirus vaccines may cause Long Covid–like symptoms | Science | AAAS).
The PEGylation of the COVID vaccine, or the formation of Virus-like particles means that instead of potentially being trapped in the liver, they escape removal by the liver and hence are trophic for the lung. In deed, PEGylation is a technology specifically designed to avoid the reticuloendothelial system, and hence avoid clearance by the liver (Wang et al, 2022; Jokerst etal, 2011; Kim etal, 2024)
Development of Pseudoexfoliation Syndrome following COVID vaccination
At least one case of Pseudoexfoliation Syndrome leading to potential blindness has been described following the Pfizer vaccine (Russell-Jones 2024)
Faulty Coating on Pfizer and Moderna vaccines
For some unknown reason the Pfizer and Moderna vaccines were formed within lipid nanoparticles (which is a standard way of protecting the mRNA), which were coated with PEG. The PEG coating is used when one wants to avoid the immune response, and dramatically changes the biodistribution of the particles, so instead of targeting the immune system, which is desirable in a vaccine, they have deliberately avoided the immune system. This would appear to be the most likely reason for the numerous Long Vax symptoms, and also why the particles have caused such a dramatic deficiency in vitamin B2, iron, and vitamin B12 in the above example. This, though is representative of data, and is similar to other data that we have for others, who were not so fortunate as to have normal metabolism prior to vaccination. In summary the particles should not have been coated with PEG. In addition, PEG has also been shown to be a major cause of anaphylaxis to the Pfizer and Moderna vaccines (Sellaturay etal, 2021), which is not surprising considering the high rate of allergy to PEG (7% Yang, et al, 2016). Despite all these problems the Therapeutic Goods Association in Australia, and so many National Medical Associations, approved the use of the vaccine!!
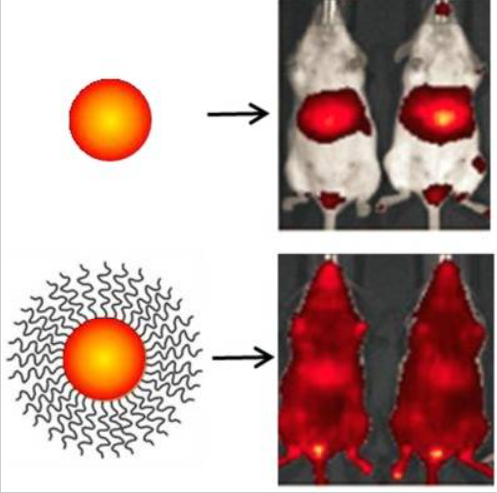
Biodistribution of uncoated fluorescent Nanoparticles (top) compared to PEG-coated Nanoparticles (Bottom) (Suk etal, 2016)
References
Wang C, Xie J, Zhao L, Fei X, Zhang H, Tan Y, Nie X, Zhou L, Liu Z, Ren Y, Yuan L, Zhang Y, Zhang J, Liang L, Chen X, Liu X, Wang P, Han X, Weng X, Chen Y, Yu T, Zhang X, Cai J, Chen R, Shi ZL, Bian XW. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine. 2020 Jul;57:102833. doi: 10.1016/j.ebiom.2020.102833. Epub 2020 Jun 20. PMID: 32574956; PMCID: PMC7305897.
Covid and ACE-2 receptors: https://www1.racgp.org.au/newsgp/clinical/ace-inhibitors-arbs-and-covid-19-what-gps-need-to?feed=RACGPnewsGPArticles
Wu etal Melatonin receptor agonist protects against acute lung injury induced by ventilator through up-regulation of IL-10 production. Resp Res (2020)
Wheatley C. A Scarlet pimpernel for the resolution of inflammation? The role of supra-therapeutic doses of cobalamin, in the treatment of Systemic Inflammatory Response Syndrome (SIRS), Sepsis, severe Sepsis and Septic or Traumatic Shock. Med Hypoth 2006 67, 134-42
Seko etal, Inhibition of angiotensin-converting enzyme by selenoneine. Fisheries Science, 2019 85, 731-736
Manzanares and Hardy. Vitamin B12: the forgotten micronutrient for critical care. Curr Opin Clin Nutr Metab Care, 2010 13, 662-8
Hoffmann and Berry. The influence of selenium on immune responses. Mol Nutr Food Res 2008, 52, 1273-1280 https://www.ncbi.nlm.nih.gov/pubmed/18384097
Beck MA, Levander OA, Handy J. (2003) Selenium deficiency and viral infection. J Nutr. 133:1463S-1467S.
https://www.ncbi.nlm.nih.gov/pubmed/12730444Beck etal. Selenium deficiency increases the pathology of an influenza virus infection. FASEB J 2001 15; 1481-3
Beck etal Benign human enterovirus becomes virulent in Selenium deficient mice. J. Med Virol 1994 43; 166-70
Chandrupatla DMSH, Jansen G, Mantel E, Low PS, Matsuyama T, Musters RP, Windhorst AD, Lammertsma AA, Molthoff CFM, van der Laken CJ. Imaging and Methotrexate Response Monitoring of Systemic Inflammation in Arthritic Rats Employing the Macrophage PET Tracer [18F]Fluoro-PEG-Folate. Contrast Media Mol Imaging. 2018 Feb 21;2018:8092781. doi: 10.1155/2018/8092781. PMID: 29681783; PMCID: PMC5841060.
Frigerio B, Bizzoni C, Jansen G, Leamon CP, Peters GJ, Low PS, Matherly LH, Figini M. Folate receptors and transporters: biological role and diagnostic/therapeutic targets in cancer and other diseases. J Exp Clin Cancer Res. 2019 Mar 12;38(1):125. doi: 10.1186/s13046-019-1123-1. PMID: 30867007; PMCID: PMC6417013.
Moisio O, Palani S, Virta J, Elo P, Liljenbäck H, Tolvanen T, Käkelä M, Miner MG, Herre EA, Marjamäki P, Örd T, Heinäniemi M, Kaikkonen MU, Zhang F, Srinivasarao M, Knuuti J, Low PS, Saraste A, Li XG, Roivainen A. Radiosynthesis and preclinical evaluation of [68Ga]Ga-NOTA-folate for PET imaging of folate receptor β-positive macrophages. Sci Rep. 2020 Aug 12;10(1):13593. doi: 10.1038/s41598-020-70394-3. PMID: 32788595; PMCID: PMC7423886.
Jahandideh A, Uotila S, Ståhle M, Virta J, Li XG, Kytö V, Marjamäki P, Liljenbäck H, Taimen P, Oikonen V, Lehtonen J, Mäyränpää MI, Chen Q, Low PS, Knuuti J, Roivainen A, Saraste A. Folate Receptor β-Targeted PET Imaging of Macrophages in Autoimmune Myocarditis. J Nucl Med. 2020 Nov;61(11):1643-1649. doi: 10.2967/jnumed.119.241356. Epub 2020 Apr 13. PMID: 32284397.
Yi YS. Folate Receptor-Targeted Diagnostics and Therapeutics for Inflammatory Diseases. Immune Netw. 2016 Dec;16(6):337-343. doi: 10.4110/in.2016.16.6.337. Epub 2016 Dec 22. PMID: 28035209; PMCID: PMC5195843.
Muller C. Folate based radiopharmaceuticals for imaging and therapy of cancer and inflammation. Curr Pharm Des. 2012;18(8):1058-83. doi: 10.2174/138161212799315777. PMID: 22272825.
Seetharam B. Upregulation of transcobalamin (TC) and its receptor in colonic inflammation: effect of homocysteine. Am J Physiol Gastrointest Liver Physiol. 2007 Oct;293(4):G918. doi: 10.1152/ajpgi.00017.2007. Epub 2007 Jul 19. PMID: 17640980.
Rabinowitz R, Rachmilewitz B, Rachmilewitz M, Schlesinger M. Production of transcobalamin II by various murine and human cells in culture. Isr J Med Sci. 1982 Jul;18(7):740-5. PMID: 7107216.
Melmed RN, Rachmilewitz B, Schneider A, Rachmilewitz M. The modulation of transcobalamin II (TC-II) production by cyclic adenosine 3',5'-monophosphate in the murine macrophage cell line J774: relationship to growth behavior. J Cell Physiol. 1986 Mar;126(3):430-4. doi: 10.1002/jcp.1041260314. PMID: 3005344.
Rosário C, Zandman-Goddard G, Meyron-Holtz EG, D'Cruz DP, Shoenfeld Y. The hyperferritinemic syndrome: macrophage activation syndrome, Still's disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med. 2013 Aug 22;11:185. doi: 10.1186/1741-7015-11-185. PMID: 23968282; PMCID: PMC3751883.
Zhou C, Chen Y, Ji Y, He X, Xue D. Increased Serum Levels of Hepcidin and Ferritin Are Associated with Severity of COVID-19. Med Sci Monit. 2020 Sep 26;26:e926178. doi: 10.12659/MSM.926178. PMID: 32978363; PMCID: PMC7526336.
Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017 Nov 1;29(9):401-409. doi: 10.1093/intimm/dxx031. PMID: 28541437; PMCID: PMC5890889.
Mahroum N, Alghory A, Kiyak Z, Alwani A, Seida R, Alrais M, Shoenfeld Y. Ferritin - from iron, through inflammation and autoimmunity, to COVID-19. J Autoimmun. 2022 Jan;126:102778. doi: 10.1016/j.jaut.2021.102778. Epub 2021 Dec 6. PMID: 34883281; PMCID: PMC8647584.
Ruscitti P, Giacomelli R. Ferritin and Severe COVID-19, from Clinical Observations to Pathogenic Implications and Therapeutic Perspectives. Isr Med Assoc J. 2020 Aug;22(8):516-518. PMID: 33236586.
Raman N, Kv P, Ashta KK, Vardhan V, Thareja S, J M, Kumar A, Basavaraj. Ferritin and Hemoglobin as Predictors of Fatal Outcome in COVID-19: Two Sides of the Same Coin. J Assoc Physicians India. 2021 Aug;69(8):11-12. PMID: 34472812. https://pubmed.ncbi.nlm.nih.gov/34472812/
Iftikhar R, Kamran SM, Mirza ZE, Naseem A, Ali Shah SA, Riaz S, Fazal I, Alamgir W, Saeed F, Saleem S, Ali RS, Chaudhry QUN. Haematological Parameters And Outcome In Hospitalized Patients With Covid-19: A Developing Country Experience. J Ayub Med Coll Abbottabad. 2021 Jul-Sep;33(3):416-424. PMID: 34487649. https://pubmed.ncbi.nlm.nih.gov/34487649/
Mohiuddin Chowdhury ATM, Karim MR, Mehedi HH, Shahbaz M, Chowdhury MW, Dan G, He S. Analysis of the primary presenting symptoms and hematological findings of COVID-19 patients in Bangladesh. J Infect Dev Ctries. 2021 Mar 7;15(2):214-223. doi: 10.3855/jidc.13692. PMID: 33690203. https://pubmed.ncbi.nlm.nih.gov/33690203/
Guo L, Lu MP, Dong GJ, Teng LP, Xu YP, Zou LX, Zheng Q. [Clinical and laboratory features of macrophage activation syndrome]. Zhongguo Dang Dai Er Ke Za Zhi. 2017 Feb;19(2):188-192. Chinese. doi: 10.7499/j.issn.1008-8830.2017.02.012. PMID: 28202118; PMCID: PMC7389461.
Keskin A, U Ustun G, Aci R, Duran U. Homocysteine as a marker for predicting disease severity in patients with COVID-19. Biomark Med. 2022 May;16(7):559-568. doi: 10.2217/bmm-2021-0688. Epub 2022 Mar 28. PMID: 35343243.
Ponti G, Ruini C, Tomasi A. Homocysteine as a potential predictor of cardiovascular risk in patients with COVID-19. Med Hypotheses. 2020 Oct;143:109859. doi: 10.1016/j.mehy.2020.109859. Epub 2020 May 21. PMID: 32464494; PMCID: PMC7240252. Carpenè G, Negrini D, Henry BM, Montagnana M, Lippi G. Homocysteine in coronavirus disease (COVID-19): a systematic literature review. Diagnosis (Berl). 2022 Jun 16. doi: 10.1515/dx-2022-0042. Epub ahead of print. PMID: 35704707.
Ponti G, Roli L, Oliva G, Manfredini M, Trenti T, Kaleci S, Iannella R, Balzano B, Coppola A, Fiorentino G, Ozben T, Paoli VD, Debbia D, De Santis E, Pecoraro V, Melegari A, Sansone MR, Lugara M, Tomasi A. Homocysteine (Hcy) assessment to predict outcomes of hospitalized Covid-19 patients: a multicenter study on 313 Covid-19 patients. Clin Chem Lab Med. 2021 Mar 26;59(9):e354-e357. doi: 10.1515/cclm-2021-0168. PMID: 33768762.
Steinbrenner H, Al-Quraishy S, Dkhil MA et al. (2015) Dietary selenium in adjuvant therapy of viral and bacterial infections. Adv Nutr. 6:73-82. https://www.ncbi.nlm.nih.gov/pubmed/25593145.
Hurwitz etal. Suppression of human immunodeficiency virus type 1 viral load with Selenium supplementation... Arch Int Med, 2007, 167, 148-54
Baum etal. High risk of HIV-related mortality is associated with selenium deficiency. J Acquir Immune Defic Syndr Hum Retrovirol 1997 15; 370-4
Zhang etal, 2016 Decreased levels of vitamin B12 in aging, autism and schizophrenia. PMID: 26799654
Escames etal. Pharmacological utility of melatonin in the treatment of septic shock: Experimental and clinical evidence. J Pharm. Pharmacol. 2006a 58: 1153-65
Lopez etal Identification of an inducible nitric oxide synthase in diaphragm mitochondria from septic mice.... Int J Biochem Cell Biol 2006b 38, 267-78
Carrillo-Vico etal. Beneficial peleotropic actions of melatonin in an experimental model of septic shock in mice.... J Pineal Res 2005 39, 400-8
Srinivasan etal. Melatonin in septic shock: some recent concepts. J Crit Care 2010 25, 656e
Reiter etal Free redical-mediated molecular damage. Mechanisms for the protective actions of melatonin in the central nervous system. Ann NYAS 2001, 939, 200-15
Reiter etal Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas. Cell Mol Life Sci 2017 74, 3863-3881
Biancatelli etal. Melatonin for the treatment of sepsis: the scientific rational. J Thorac Dis 2020 12: S54-S65
Favero etal Melatonin as an Anti-inflammatory agent modulating inflammasome activation. Int J Endocrinol. 2017 2017:1835195
Abgstrwurm etal Selenium in Intensive care..... Crit Care Med 2007 35, 118-26
Kurniawan etal. Glutathione restricts serine metabolism to preserve regulatory T cell function. Cell metabolism. 2020, doi.org/10.1015/j.cmet.2020.03.004
Carnesecchi etal NADPH Oxidase-1 plays a crucial Role in Hyperoxia-induced acute lung injury in mice 2009. rccm.200902-0296OC
Bailey etal. The epidemiology of global micronutrient deficiencies. Ann Nutr Metab. 2015 66; 22-33
Stepan etal. Implications of the iron deficiency in lower tract respiratory acute infections in toddlers. Curr Health Sci J. 2018 44; 362-367
Tansarli etal Iron deficiency and susceptibility to infections: Evaluation of the clinical evidence. Eur J. Clin Microbiol Infect Dis. 2013, 32; 1253-8
Bai etal . Clinical characteristics of 14 critically ill children with 2009 Infuenza A (H1N1). Zhonghua Er Ke Za Zhi 2010 48; 860-4
Lakhan etal Retrospective review of factors associated with severe hospitalised community-acquired influenza... Inf Other Resp Vir 2016, 10; 476-485
Nickol etal. A cross-sectional study of the prevalence and associations of iron deficiency in a cohort of patients with chronic obstructive pulmonary disease. BMJ Open 2015 5 e007911
De Silva etal. Iron supplementation improves iron status and reduces morbidity in children with or without upper respiratory tract infections:.. Am J Clin Nutr 2003 77; 234-41.
Yu etal. A review of the novel application and potential adverse effects of proton pump inhibitors. Adv Ther 2017 34, 1070-1086
Hurrell RF Iron fortification: its efficacy and safety in relation to infections. Food Nutr Bull 2007 29, S585-94
Semba RD. Vitamin A and immunity to viral, bacterial and protozoan infections. Proc Nutr Soc 1999, 58; 385-392
Lee etal. Effects of dietary vitamin A content on antibody responses of feed-lot calves inoculated intramuscularly with an inactivated bovine coronavirus vaccine. Am J Vet Res 2013, 75;1353-1352
Hemila H. itamin C and SARS coronavirus. J Antimicrob Chemother 2003, 52:1049-50
Atherton etal. The effect of ascorbic acid on infection chick-embro ciliated trachael organ cultures by coronavirus. Arch Virol. 1978; 56, 195-199
Nonnecke etal, 2014; 97, 5566-5579.
Zhang et al. COVID-19; Melatonin as a potential adjuvant treatment Life Sci
Zhang etal. Association between regional Selenium status and reported outcome of COVID-19 cases in China. Am J Clin Nut
(thanks to J Frick)Reiter etal, 2020 https://www.frontiersin.org/articles/10.3389/fmed.2020.00226/full?fbclid=IwAR1Ol2f5qqWAJJTUS4biFzQw3xQnzdridTi22BLXtRVRmZOALeTI2zhRc2U#F2
Zhang and Liu Potential interventions for novel coronavirus in China: A systematic review. J Med Virol 2020 https://doi.org/10.1002/jmv.25707
Rayman etal. Association between regional selenium status and reported outcome of COVID-19 cases in China. Am J. Clin Nut 2020.DOI: 10.1093/ajcn/nqaa095
Carnesecchi etal Martineau etal Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 2017 346
Parinandi etal. Hyperoxia-induced NAD(P)H oxidase activation and regulation by map kinases in human lung endothelial cells. Am J. Physiol 284: 128 - L26-28
Ginde etal. Association between serum 25-hyroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 2009 169:384-390
Joliffe etal, Vitamin D in the prevention of acute respiratory infection. Systematic review of clinical studies. J Steroid Biochem Mol Biol 2013; 136, 321-329
Bjelakovic etal Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Sys Rev. 2011 PMID 21735411
Evidence that vitamin D supplementation could reduce the risk of Influenza and COVID-19 infections and death https://www.ncbi.nlm.nih.gov/pubmed/32252338
Sizar etal Vitamin D Deficiency 2020 https://www.ncbi.nlm.nih.gov/books/NBK532266/
https://www.ncbi.nlm.nih.gov/21310306
Ireland Vitamin D https://tildo.tcd.ie/publications/reports/pdf/Report_Covid19VitaminD.pdf
John Campbell Utube discussion https://www.youtube.com/watch?v=GCSXNGc7pfs&t=1s
https://www.research.square.com/article/rr-21211/v1
https://www.ncbi.nlm.nih.gov/pmc/article/PMC5954269/
Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the
severity of COVID-19? Clin Med (Lond). 2020 Jul;20(4):e107-e108. doi:
10.7861/clinmed.2020-0301. Epub 2020 Jun 5.
PMID: 32503801 Free PMC article.
De Smet D, De Smet K, Herroelen P, Gryspeerdt S, Martens GA.Serum 25(OH)D Level
on Hospital Admission Associated With COVID-19 Stage and Mortality. Am J Clin
Pathol. 2021 Feb 11;155(3):381-388. doi: 10.1093/ajcp/aqaa252.
PMID: 33236114 Free PMC article.
Xu Y, Baylink DJ, Chen CS, Reeves ME, Xiao J, Lacy C, Lau E, Cao H. The
importance of vitamin d metabolism as a potential prophylactic, immunoregulatory
and neuroprotective treatment for COVID-19. J Transl Med. 2020 Aug 26;18(1):322.
doi: 10.1186/s12967-020-02488-5.
PMID: 32847594 Free PMC article. Review.
Skulachev, VP. Possible role of reactive oxygen species in antiviral defense. Biochemistry (Mosc). 1998 Dec: 63912):1438-40 PMIDP9916163
Pizzini A, Aichner M, Sahanic S, Böhm A, Egger A, Hoermann G, Kurz K, Widmann G,
Bellmann-Weiler R, Weiss G, Tancevski I, Sonnweber T, Löffler-Ragg J. Impact of
Vitamin D Deficiency on COVID-19-A Prospective Analysis from the CovILD
Registry. Nutrients. 2020 Sep 11;12(9):2775. doi: 10.3390/nu12092775. PMID:
32932831 Free PMC article.
Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and
severity. J Infect Public Health. 2020 Oct;13(10):1373-1380. doi:
10.1016/j.jiph.2020.06.021. Epub 2020 Jun 20. PMID: 32605780 Free PMC article.
N Basaran, M Adas, Y Gokden, N Turgut, T Yildirmak, G Guntas The relationship between vitamin D and the severity of COVID-19 Bratisl Lek Listy 2021;122(3):200-205. doi: 10.4149/BLL_2021_034. PMID: 33618529 DOI: 10.4149/BLL_2021_034
Feng etal 2020 https://www.biorxiv.org/content/10.1101/2020.03.03.962332v1.full.pdf
Bok etal, Passive immunity to control bovine coronavirus diarrhea in a dairy herd in Argentina. Reve Argent Micobiol 2018 51, 23-30.
Moderna https://time.com/5790545/first-covid-19-vaccine/
CDC https://www.cdc.gov/flu/about/burden/index.html
Iuliano etal Estimates of global seasonal Influenza - Associated respirator Mortality: A modelling study. Lancet 2018, 391; 1285-1300 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5935243/pdf/nihms962240.pdf
Barouch. Monkey vaccine trial 2020 https://www.msn.com/en-au/news/world/monkeys-resist-virus-re-infection-after-vaccine-study-immunisation/ar-BB14qGad?ocid=spartanntp
Giustina etal, 2020 https://www.bmj.com/content/368/bmj.m810/rr-36
Garami 2020 https://www.bmj.com/content/368/bmj.m810/rr-24
Caly etal, The FDA-approved drug Ivermectin inhibits the replication of SARS-CoV-2 in vitro. https://www.sciencedirect.com/science/article/pii/S0166354220302011
Yang etal 2016 Factors influencing immunologic response to hepatitis B vaccine in adults https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914839/pdf/srep27251.pdf
Kim etal, Relationship between serum vitamin D concentrations and clinical outcome of community-acquired pneumonia.Int J Tuberc Lung Dis 2015 19: 729-34 PMID 25946368
Remmelts etal. Addition of vitamin D status to prognostic scores improves the prediction of outcome in community-acquired pneumonia. Clin Infect Dis 2012 55:1488-94 PMID 22942205
Leow etal 2011 Vitamin D, innate immunity and outcomes in community acquired pneumonia. Respirology 2011 16: 611-6 PMID 21244571
Mathias etal. Vitamin D deficiency in community-acquired pneumonia: Low levels of 1,25(OH)2 D are associated with disease severity. Respir Res. 2014 15-53
Vitamin D to be added to M&S bread https://www.bbc.com/news/uk-32941923
Vitamin D recommendations by UK health https://www.gov.uk/government/news/phe-publishes-new-advice-on-vitamin-d
McCaddon and Regland COVID-19: A methyl group assaults? Medical Hypotheses 149, 2021; 110543
Nielsen, N.M., Junker, T.G., Boelt, S.G. et al. Vitamin D status and severity of COVID-19. Sci Rep 12, 19823 (2022). https://doi.org/10.1038/s41598-022-21513-9
Luigi di Filippo, Stefano Frara, Fabrizio Nannipieri, Alice Cotellessa, Massimo Locatelli, Patrizia Rovere Querini, Andrea Giustina, Low Vitamin D Levels Are Associated With Long COVID Syndrome in COVID-19 Survivors, The Journal of Clinical Endocrinology & Metabolism, Volume 108, Issue 10, October 2023, Pages e1106–e1116, https://doi.org/10.1210/clinem/dgad207
Klaser K, Thompson EJ, Nguyen LH, Sudre CH, Antonelli M, Murray B, Canas LS, Molteni E, Graham MS, Kerfoot E, Chen L, Deng J, May A, Hu C, Guest A, Selvachandran S, Drew DA, Modat M, Chan AT, Wolf J, Spector TD, Hammers A, Duncan EL, Ourselin S, Steves CJ. Anxiety and depression symptoms after COVID-19 infection: results from the COVID Symptom Study app. J Neurol Neurosurg Psychiatry. 2021 Dec;92(12):1254-1258. doi: 10.1136/jnnp-2021-327565. Epub 2021 Sep 28. PMID: 34583944; PMCID: PMC8599635.
Piazza M, Di Cicco M, Pecoraro L, Ghezzi M, Peroni D, Comberiati P. Long COVID-19 in Children: From the Pathogenesis to the Biologically Plausible Roots of the Syndrome. Biomolecules. 2022 Apr 8;12(4):556. doi: 10.3390/biom12040556. PMID: 35454144; PMCID: PMC9024951.
COVID-19 Lung Damage | Johns Hopkins Medicine
How coronavirus kickstarts deadly lung inflammation - Futurity
Study sheds light on mysterious post-COVID inflammatory syndrome in adults called MIS-A | NHLBI, NIH
COVID-19 Pneumonia: Symptoms, Treatment & Recovery (clevelandclinic.org)
Covid-19 infections can set off massive inflammation in the body | CNN
What drives severe lung inflammation in COVID-19? (medicalxpress.com)
Protracted inflammation linked to post-COVID lung problems (medicalxpress.com)
Long COVID symptoms linked to inflammation | National Institutes of Health (NIH)
Booz, G. W., Altara, R., Eid, A. H., Wehbe, Z., Fares, S., Zaraket, H., Habeichi, N. J., & Zouein, F. A. (2020). Macrophage responses associated with COVID-19: A pharmacological perspective. European journal of pharmacology, 887, 173547. https://doi.org/10.1016/j.ejphar.2020.173547
Sefik E, Qu R, Junqueira C, Kaffe E, Mirza H, Zhao J, Brewer JR, Han A, Steach HR, Israelow B, Blackburn HN, Velazquez SE, Chen YG, Halene S, Iwasaki A, Meffre E, Nussenzweig M, Lieberman J, Wilen CB, Kluger Y, Flavell RA. Inflammasome activation in infected macrophages drives COVID-19 pathology. Nature. 2022 Jun;606(7914):585-593. doi: 10.1038/s41586-022-04802-1. Epub 2022 Apr 28. PMID: 35483404; PMCID: PMC9288243.
Wang X, Liu S, Sun Y, Yu X, Lee SM, Cheng Q, Wei T, Gong J, Robinson J, Zhang D, Lian X, Basak P, Siegwart DJ. Preparation of selective organ-targeting (SORT) lipid nanoparticles (LNPs) using multiple technical methods for tissue-specific mRNA delivery. Nat Protoc. 2023 Jan;18(1):265-291. doi: 10.1038/s41596-022-00755-x. Epub 2022 Oct 31. PMID: 36316378; PMCID: PMC9888002.
Jokerst JV, Lobovkina T, Zare RN, Gambhir SS. Nanoparticle PEGylation for imaging and therapy. Nanomedicine (Lond). 2011 Jun;6(4):715-28. doi: 10.2217/nnm.11.19. PMID: 21718180; PMCID: PMC3217316.
Kim J, Eygeris Y, Ryals RC, Jozić A, Sahay G. Strategies for non-viral vectors targeting organs beyond the liver. Nat Nanotechnol. 2024 Apr;19(4):428-447. doi: 10.1038/s41565-023-01563-4. Epub 2023 Dec 27. PMID: 38151642.
Fakhri S, Abbaszadeh F, Dargahi L, Pouriran R, Jorjani M. Astaxanthin ameliorates serum level and spinal expression of macrophage migration inhibitory factor following spinal cord injury. Behav Pharmacol. 2022 Oct 1;33(7):505-512. doi: 10.1097/FBP.0000000000000698. Epub 2022 Sep 14. PMID: 36148838.
Fakhri S, Nouri Z, Moradi SZ, Farzaei MH. Astaxanthin, COVID-19 and immune response: Focus on oxidative stress, apoptosis and autophagy. Phytother Res. 2020 Nov;34(11):2790-2792. doi: 10.1002/ptr.6797. Epub 2020 Aug 4. PMID: 32754955; PMCID: PMC7436866.
Park MD. Macrophages: a Trojan horse in COVID-19? Nat Rev Immunol. 2020 Jun;20(6):351. doi: 10.1038/s41577-020-0317-2. PMID: 32303696; PMCID: PMC7186930.
Percivalle E, Sammartino JC, Cassaniti I, Arbustini E, Urtis M, Smirnova A, Concardi M, Belgiovine C, Ferrari A, Lilleri D, Piralla A, Baldanti F. Macrophages and Monocytes: "Trojan Horses" in COVID-19. Viruses. 2021 Oct 28;13(11):2178. doi: 10.3390/v13112178. PMID: 34834984; PMCID: PMC8624282.
Farruggia C, Kim MB, Bae M, Lee Y, Pham TX, Yang Y, Han MJ, Park YK, Lee JY. Astaxanthin exerts anti-inflammatory and antioxidant effects in macrophages in NRF2-dependent and independent manners. J Nutr Biochem. 2018 Dec;62:202-209. doi: 10.1016/j.jnutbio.2018.09.005. Epub 2018 Sep 19. PMID: 30308382.
Li W, Hellsten A, Jacobsson LS, Blomqvist HM, Olsson AG, Yuan XM. Alpha-tocopherol and astaxanthin decrease macrophage infiltration, apoptosis and vulnerability in atheroma of hyperlipidaemic rabbits. J Mol Cell Cardiol. 2004 Nov;37(5):969-78. doi: 10.1016/j.yjmcc.2004.07.009. PMID: 15522274.
Liu F, Smith AD, Solano-Aguilar G, Wang TTY, Pham Q, Beshah E, Tang Q, Urban JF Jr, Xue C, Li RW. Mechanistic insights into the attenuation of intestinal inflammation and modulation of the gut microbiome by krill oil using in vitro and in vivo models. Microbiome. 2020 Jun 4;8(1):83. doi: 10.1186/s40168-020-00843-8. PMID: 32498703; PMCID: PMC7273679.
Santos SD, Cahú TB, Firmino GO, de Castro CC, Carvalho LB Jr, Bezerra RS, Filho JL. Shrimp waste extract and astaxanthin: rat alveolar macrophage, oxidative stress and inflammation. J Food Sci. 2012 Jul;77(7):H141-6. doi: 10.1111/j.1750-3841.2012.02762.x. PMID: 22757706.
Chen Y , Tie S , Zhang X , Zhang L , Tan M . Preparation and characterization of glycosylated protein nanoparticles for astaxanthin mitochondria targeting delivery. Food Funct. 2021 Sep 7;12(17):7718-7727. doi: 10.1039/d1fo01751a. Epub 2021 Jul 21. PMID: 34286807.
Mamun-Or-Rashid ANM, Lucy TT, Yagi M, Yonei Y. Inhibitory Effects of Astaxanthin on CML-HSA-Induced Inflammatory and RANKL-Induced Osteoclastogenic Gene Expression in RAW 264.7 Cells. Biomedicines. 2021 Dec 27;10(1):54. doi: 10.3390/biomedicines10010054. PMID: 35052734; PMCID: PMC8772757.
Kang H, Lee Y, Bae M, Park YK, Lee JY. Astaxanthin inhibits alcohol-induced inflammation and oxidative stress in macrophages in a sirtuin 1-dependent manner. J Nutr Biochem. 2020 Nov;85:108477. doi: 10.1016/j.jnutbio.2020.108477. Epub 2020 Aug 12. PMID: 32801029.
Zhu L, Wu H, Ma Z, Dong D, Yang Z, Tian J. Astaxanthin ameliorates lipopolysaccharide-induced acute lung injury inhibition of inflammatory reactions and modulation of the SOCS3/JAK2/STAT3 signaling pathways in mice. Food Funct. 2022 Nov 14;13(22):11638-11651. doi: 10.1039/d2fo02182j. PMID: 36278420.
Cai X, Chen Y, Xie X, Yao D, Ding C, Chen M. Astaxanthin prevents against lipopolysaccharide-induced acute lung injury and sepsis via inhibiting activation of MAPK/NF-κB. Am J Transl Res. 2019 Mar 15;11(3):1884-1894. Erratum in: Am J Transl Res. 2021 Jun 15;13(6):7420-7421. PMID: 30972212; PMCID: PMC6456544.
COVID and Homocysteine
Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020 Sep;57(6):389-399. doi: 10.1080/10408363.2020.1770685. Epub 2020 Jun 5. PMID: 32503382; PMCID: PMC7284147.
Perła-Kaján J, Jakubowski H. COVID-19 and One-Carbon Metabolism. Int J Mol Sci. 2022 Apr 10;23(8):4181. doi: 10.3390/ijms23084181. PMID: 35456998; PMCID: PMC9026976.
Koklesova L, Mazurakova A, Samec M, Biringer K, Samuel SM, Büsselberg D, Kubatka P, Golubnitschaja O. Homocysteine metabolism as the target for predictive medical approach, disease prevention, prognosis, and treatments tailored to the person. EPMA J. 2021 Nov 11;12(4):477-505. doi: 10.1007/s13167-021-00263-0. PMID: 34786033; PMCID: PMC8581606.
Fouda EM, Wahba NS, Elsharawy AIM, Ishak SR. Serum homocysteine level in pediatric patients with COVID-19 and its correlation with the disease severity. Pediatr Pulmonol. 2022 Jul;57(7):1701-1708. doi: 10.1002/ppul.25920. Epub 2022 Apr 22. PMID: 35420248; PMCID: PMC9088336.
Abu-Farha M, Al-Sabah S, Hammad MM, Hebbar P, Channanath AM, John SE, Taher I, Almaeen A, Ghazy A, Mohammad A, Abubaker J, Arefanian H, Al-Mulla F, Thanaraj TA. Prognostic Genetic Markers for Thrombosis in COVID-19 Patients: A Focused Analysis on D-Dimer, Homocysteine and Thromboembolism. Front Pharmacol. 2020 Dec 9;11:587451. doi: 10.3389/fphar.2020.587451. PMID: 33362545; PMCID: PMC7756688.
Batista KS, Cintra VM, Lucena PAF, Manhães-de-Castro R, Toscano AE, Costa LP, Queiroz MEBS, de Andrade SM, Guzman-Quevedo O, Aquino JS. The role of vitamin B12 in viral infections: a comprehensive review of its relationship with the muscle-gut-brain axis and implications for SARS-CoV-2 infection. Nutr Rev. 2022 Feb 10;80(3):561-578. doi: 10.1093/nutrit/nuab092. PMID: 34791425; PMCID: PMC8689946.
Wee AKH. COVID-19's toll on the elderly and those with diabetes mellitus - Is
vitamin B12 deficiency an accomplice? Med Hypotheses. 2021 Jan;146:110374. doi:
10.1016/j.mehy.2020.110374. Epub 2020 Nov 12. PMID: 33257090; PMCID: PMC7659645.
Hayden MR, Tyagi SC. Impaired Folate-Mediated One-Carbon Metabolism in Type 2
Diabetes, Late-Onset Alzheimer's Disease and Long COVID. Medicina (Kaunas). 2021
Dec 23;58(1):16. doi: 10.3390/medicina58010016. PMID: 35056324; PMCID:
PMC8779539.
Carpenè G, Negrini D, Henry BM, Montagnana M, Lippi G. Homocysteine in
coronavirus disease (COVID-19): a systematic literature review. Diagnosis (Berl).
2022 Jun 16;9(3):306-310. doi: 10.1515/dx-2022-0042. PMID: 35704707.
McCaddon A, Regland B. COVID-19: A methyl-group assault? Med Hypotheses.
2021 Apr;149:110543. doi: 10.1016/j.mehy.2021.110543. Epub 2021 Feb 18. PMID:
33657459; PMCID: PMC7890339.
Keskin A, U Ustun G, Aci R, Duran U. Homocysteine as a marker for predicting
disease severity in patients with COVID-19. Biomark Med. 2022 May;16(7):559-568.
doi: 10.2217/bmm-2021-0688. Epub 2022 Mar 28. PMID: 35343243.
Ponti G, Pastorino L, Manfredini M, Ozben T, Oliva G, Kaleci S, Iannella R,
Tomasi A. COVID-19 spreading across world correlates with C677T allele of the
methylenetetrahydrofolate reductase (MTHFR) gene prevalence. J Clin Lab Anal.
2021 Jul;35(7):e23798. doi: 10.1002/jcla.23798. Epub 2021 Jun 1. PMID: 34061414;
PMCID: PMC8209953.
Wu G, Wang S, Wang T, Han J, Yu A, Feng C, Wang Y, Liu S. Neurological and Psychological Characteristics of Young Nitrous Oxide Abusers and Its Underlying Causes During the COVID-19 Lockdown. Front Public Health. 2022 Jun 2;10:854977. doi: 10.3389/fpubh.2022.854977. PMID: 35719623; PMCID: PMC9201030.
Ramadan H, Shennawy AM. Correlation between vitamin D level and severity of prognostic markers in Egyptian COVID-19 patients: a cohort study. Egypt J Intern Med. 2022;34(1):49. doi: 10.1186/s43162-022-00131-x. Epub 2022 Jun 22. PMID: 35754946; PMCID: PMC9214466.
Filip N, Cojocaru E, Badulescu OV, Clim A, Pinzariu AC, Bordeianu G, Jehac AE, Iancu CE, Filip C, Maranduca MA, Sova IA, Serban IL. SARS-CoV-2 Infection: What Is Currently Known about Homocysteine Involvement? Diagnostics (Basel). 2022 Dec 21;13(1):10. doi: 10.3390/diagnostics13010010. PMID: 36611302; PMCID:PMC9818222.
Mahalapbutr P, Kongtaworn N, Rungrotmongkol T. Structural insight into the recognition of <i>S</i>-adenosyl-L-homocysteine and sinefungin in SARS-CoV-2 sp16/Nsp10 RNA cap 2'-O-Methyltransferase. Comput Struct Biotechnol J. 2020;18:2757-2765. doi: 10.1016/j.csbj.2020.09.032. Epub 2020 Oct 1. PMID: 33020707; PMCID: PMC7527316.
Ponti G, Roli L, Oliva G, Manfredini M, Trenti T, Kaleci S, Iannella R, Balzano B, Coppola A, Fiorentino G, Ozben T, Paoli VD, Debbia D, De Santis E, Pecoraro V, Melegari A, Sansone MR, Lugara M, Tomasi A. Homocysteine (Hcy) assessment to predict outcomes of hospitalized Covid-19 patients: a multicenter study on 313 Covid-19 patients. Clin Chem Lab Med. 2021 Mar 26;59(9):e354-e357. doi: 10.1515/cclm-2021-0168. PMID: 33768762.
Ponti G, Ruini C, Tomasi A. Homocysteine as a potential predictor of cardiovascular risk in patients with COVID-19. Med Hypotheses. 2020 Oct;143:109859. doi: 10.1016/j.mehy.2020.109859. Epub 2020 May 21. PMID: 32464494; PMCID: PMC7240252.
Kryukov EV, Ivanov AV, Karpov VO, Vasil'evich Aleksandrin V, Dygai AM, Kruglova MP, Kostiuchenko GI, Kazakov SP, Kubatiev AA. Plasma S-Adenosylmethionine Is Associated with Lung Injury in COVID-19. Dis Markers. 2021 Dec 16;2021:7686374. doi: 10.1155/2021/7686374. PMID: 34956420; PMCID: PMC8702356.
Ibrahimagić OĆ, Smajlović D, Dostović Z, Vidović M, Tupković E, Kunić S. COMMENT ON AN ARTICLE: "Homocysteine as a potential predictor of cardiovascular risk in patients with COVID-19". Med Hypotheses. 2020 Oct;143:110107. doi: 10.1016/j.mehy.2020.110107. Epub 2020 Jul 15. PMID: 32721803; PMCID: PMC7361037.
Petelina TI, Musikhina NA, Garanina VD, Gorbatenko EA, Shcherbinina AE, Zhmurov DV, Zhmurov VA, Gapon LI, Galeeva NA, Avdeeva KS, Kapustina AA, Yaroslavskaya EI. Prospective analysis of laboratory blood parameters in patients with cardiovascular diseases who underwent COVID-19-associated pneumonia. Klin Lab Diagn. 2022 Mar 25;67(3):133-139. English. doi: 10.51620/0869-2084-2022-67-3-133-139. PMID: 35320627.
Berbert A. Further comment on articles pertaining to: "Homocysteine as a potential predictor of cardiovascular risk in patients with COVID-19". Med Hypotheses. 2021 Oct;155:110676. doi: 10.1016/j.mehy.2021.110676. Epub 2021 Sep 4. PMID: 34555782; PMCID: PMC8418050.
Kottur J, Rechkoblit O, Quintana-Feliciano R, Sciaky D, Aggarwal AK. High-resolution structures of the SARS-CoV-2 N7-methyltransferase inform therapeutic development. Nat Struct Mol Biol. 2022 Sep;29(9):850-853. doi: 10.1038/s41594-022-00828-1. Epub 2022 Sep 8. PMID: 36075969.
Chandrasekaran PR. A Curious Case of Occlusive Retinal Vasculitis in a Young Individual Associated with COVID-19 Vaccination. Ocul Immunol Inflamm. 2022 Oct 28:1-7. doi: 10.1080/09273948.2022.2137046. Epub ahead of print. PMID: 36306426.
Otava T, Šála M, Li F, Fanfrlík J, Devkota K, Perveen S, Chau I, Pakarian P, Hobza P, Vedadi M, Boura E, Nencka R. The Structure-Based Design of SARS-CoV-2 nsp14 Methyltransferase Ligands Yields Nanomolar Inhibitors. ACS Infect Dis. 2021 Aug 13;7(8):2214-2220. doi: 10.1021/acsinfecdis.1c00131. Epub 2021 Jun 21. PMID: 34152728; PMCID: PMC8265718.
Rosas-Lemus M, Minasov G, Shuvalova L, Inniss NL, Kiryukhina O, Brunzelle J, Satchell KJF. High-resolution structures of the SARS-CoV-2 2'-<i>O</i>-methyltransferase reveal strategies for structure-based inhibitor
design. Sci Signal. 2020 Sep 29;13(651):eabe1202. doi: 10.1126/scisignal.abe1202. PMID: 32994211; PMCID: PMC8028745.
Wilamowski M, Sherrell DA, Minasov G, Kim Y, Shuvalova L, Lavens A, Chard R, Maltseva N, Jedrzejczak R, Rosas-Lemus M, Saint N, Foster IT, Michalska K, Satchell KJF, Joachimiak A. 2'-O methylation of RNA cap in SARS-CoV-2 captured by serial crystallography. Proc Natl Acad Sci U S A. 2021 May
Guido CA, Lucidi F, Midulla F, Zicari AM, Bove E, Avenoso F, Amedeo I, Mancino E, Nenna R, De Castro G, Capponi M, Cinicola BL, Brindisi G, Grisoni F, Murciano M, Spalice A and the Long-Covid Group of Department of Maternal Sciences (2022) Neurological and psychological ...
Stein, M.; Ashkenazi-Hoffnung, L.; Greenberg, D.; Dalal, I.; Livni, G.; Chapnick, G.; Stein-Zamir, C.; Ashkenazi, S.; Hecht-Sagie, L.; Grossman, Z. The Burden of COVID-19 in Children and Its Prevention by Vaccination: A Joint Statement of the Israeli Pediatric Association and the Israeli Society for Pediatric Infectious Diseases. Vaccines 2022, 10, 81.
Bahrampour Juybari K, Pourhanifeh MH, Hosseinzadeh A, Hemati K, Mehrzadi S. Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Res. 2020 Oct 2;287:198108. doi: 10.1016/j.virusres.2020.198108. Epub 2020 Aug 5. PMID: 32768490; PMCID: PMC7405774.
Brown GM, Pandi-Perumal SR, Pupko H, Kennedy JL, Cardinali DP. Melatonin as an Add-On Treatment of COVID-19 Infection: Current Status. Diseases. 2021 Sep 20;9(3):64. doi: 10.3390/diseases9030064. PMID: 34562971; PMCID: PMC8482145.
Cross KM, Landis DM, Sehgal L, Payne JD. Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy. Endocr Pract. 2021 Aug;27(8):850-855. doi: 10.1016/j.eprac.2021.06.001. Epub 2021 Jun 10. PMID: 34119679; PMCID: PMC8190272.
Reardon S. Long COVID risk falls only slightly after vaccination, huge study shows. Nature. 2022 May 25. doi: 10.1038/d41586-022-01453-0. Epub ahead of print. PMID: 35614263.
I-RECOVER: Long COVID Treatment - FLCCC Alliance (covid19criticalcare.com)
Doris Loh | Doris Loh (doris-loh.com)
Loh, D.; Reiter, RJ Melatonin: Regulation of Viral Phase Separation and
Epitranscriptomics in Post-Acute Sequelae of COVID-19. Int.
J. Mol. Sci. 2022 , 23 (15),
8122. https://doi.org/10.3390/
Loh, D.; Reiter, RJ Light, Water, and Melatonin: The Synergistic Regulation of
Phase Separation in Dementia. Int.
J. Mol. Sci. 2023 , 24 ,
5835. https://doi.org/10.3390/
Kamoi K, Ohno-Matsui K. Long Vax in the Eye: Long Post-COVID Vaccination Syndrome Presenting with Frosted Branch Angiitis. Diseases. 2024 Feb 9;12(2):36. doi: 10.3390/diseases12020036. PMID: 38391783; PMCID: PMC10888280.
Finsterer J. A Case Report: Long Post-COVID Vaccination Syndrome During the Eleven Months After the Third Moderna Dose. Cureus. 2022 Dec 12;14(12):e32433. doi: 10.7759/cureus.32433. PMID: 36644105; PMCID: PMC9833629.
Lee 2022 Largest ‘Long Vax’ Study To Date On Post-Covid-19 Vaccination Syndrome (forbes.com)
Excess deaths in 2022 among worst in 50 years (bbc.com)
Excess Deaths in Australia: Frequently Asked Questions – Parliament of Australia (aph.gov.au)
AstraZeneca faces legal challenge over Covid vaccine (bbc.com)
BMJ 2023; 380 doi: https://doi.org/10.1136/bmj.p725 (Published 28 March 2023)
Re: Patients launch legal action against AstraZeneca over its covid-19 vaccine | The BMJ
AstraZeneca faces two lawsuits in London over COVID-19 vaccine | Health News | Al Jazeera
In rare cases, coronavirus vaccines may cause Long Covid–like symptoms | Science | AAAS
Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016 Apr 1;99(Pt A):28-51. doi: 10.1016/j.addr.2015.09.012. Epub 2015 Oct 9. PMID: 26456916; PMCID: PMC4798869.
Sellaturay P, Nasser S, Islam S, Gurugama P, Ewan PW. Polyethylene glycol (PEG) is a cause of anaphylaxis to the Pfizer/BioNTech mRNA COVID-19 vaccine. Clin Exp Allergy. 2021 Jun;51(6):861-863. doi: 10.1111/cea.13874. Epub 2021 Apr 9. PMID: 33825239; PMCID: PMC8251011.
Yang Q, Jacobs TM, McCallen JD, et al. Analysis of pre-existing IgG and IgM antibodies against polyethylene glycol (PEG) in the general population. Anal Chem. 2016;88(23):11804-11812. doi:10.1021/acs.analchem.6b03437
Russell-Jones G. Pseudoexfoliation Syndrome Post COVID Vaccination. J Med - Clin Res & Rev. 2024; 8(4): 1-7.. PDF